DEA for Physician Assistant: A Comprehensive Guide to Prescribing Controlled Substances
Navigating the complex world of controlled substance prescribing can be daunting for physician assistants (PAs). Understanding the Drug Enforcement Administration’s (DEA) regulations is crucial for providing safe and effective patient care while maintaining compliance. This comprehensive guide provides an in-depth exploration of the DEA requirements for PAs, offering practical insights and expert advice to ensure responsible prescribing practices. We’ll cover everything from initial registration to ongoing compliance, empowering you to confidently manage controlled substances within your practice.
This article aims to be the definitive resource on DEA regulations for PAs. Unlike other resources, we delve into the nuances of state and federal laws, offering practical guidance based on expert consensus and best practices. By the end of this guide, you will have a clear understanding of your responsibilities, minimizing the risk of non-compliance and ensuring the safety of your patients.
Understanding the DEA and Its Role in Prescribing
The Drug Enforcement Administration (DEA) is a federal law enforcement agency responsible for combating drug trafficking and abuse within the United States. Its role extends to regulating the manufacturing, distribution, and dispensing of controlled substances. For physician assistants, understanding the DEA’s regulations is paramount, as it directly impacts their ability to prescribe controlled substances legally and ethically. The DEA aims to prevent diversion and misuse of these medications, while ensuring that patients have access to necessary treatments.
The DEA categorizes drugs into five schedules based on their potential for abuse and accepted medical use. Schedule I drugs have the highest potential for abuse and no accepted medical use (e.g., heroin, LSD). Schedule II drugs have a high potential for abuse but also have accepted medical use (e.g., opioids like oxycodone and fentanyl, stimulants like amphetamine). Schedules III, IV, and V drugs have progressively lower potentials for abuse. PAs can typically prescribe Schedules II-V, but specific regulations can vary by state. Understanding these schedules is fundamental to understanding the scope of a PA’s prescribing authority.
State laws further regulate the prescribing of controlled substances. These regulations may include limitations on the types of medications that can be prescribed, the quantity of medications that can be dispensed, and the requirements for patient monitoring. It’s crucial for PAs to be aware of both federal and state laws to ensure compliance. In many cases, state laws are more restrictive than federal laws, and PAs must adhere to the stricter regulations.
DEA Registration for Physician Assistants: The Application Process
To prescribe controlled substances, a physician assistant must obtain a DEA registration. The application process involves several steps and requires careful attention to detail. Here’s a breakdown of the process:
* **Eligibility:** Verify that you meet the eligibility requirements for DEA registration. This typically includes holding a valid PA license and having prescriptive authority granted by your supervising physician and state regulations.
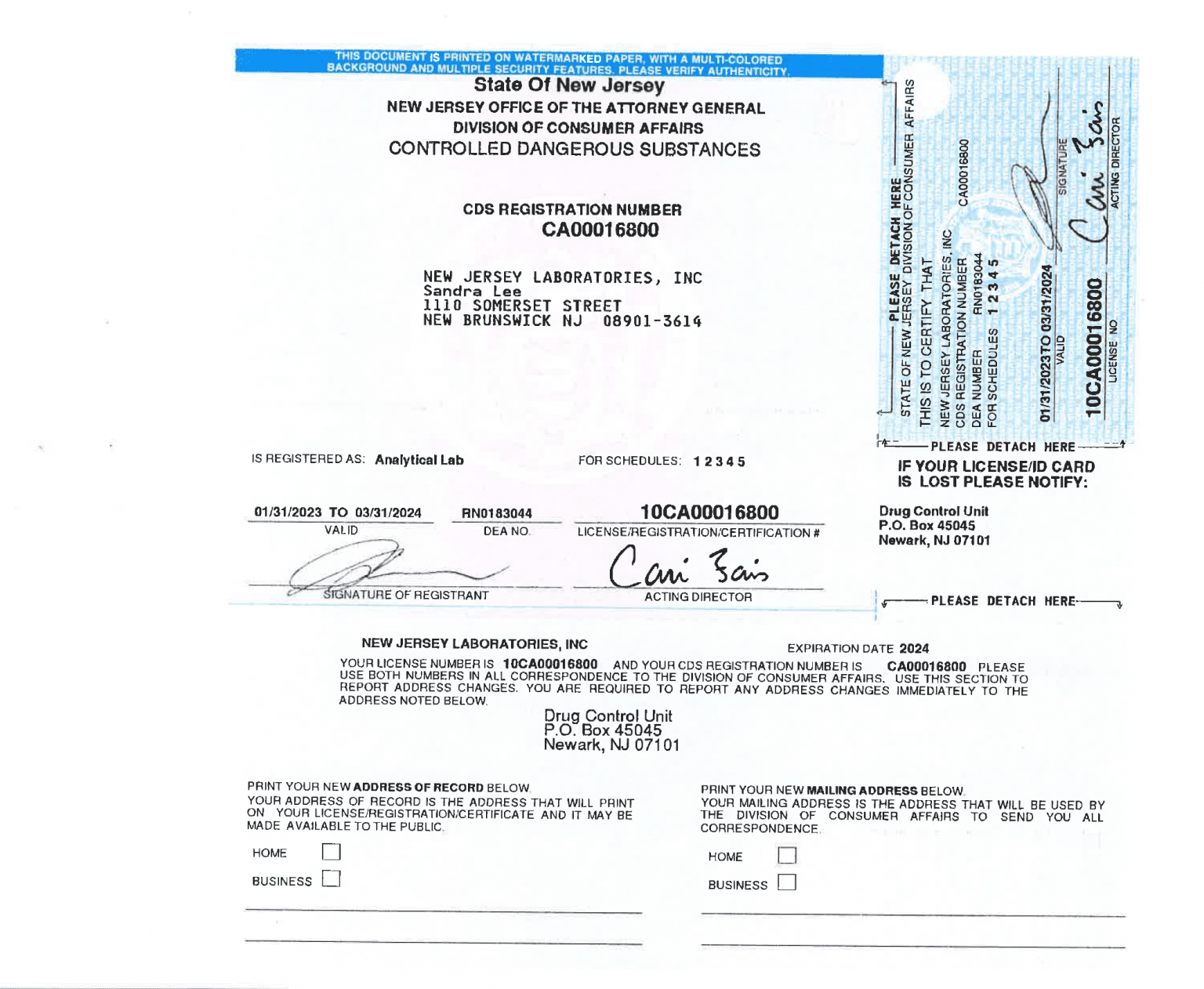
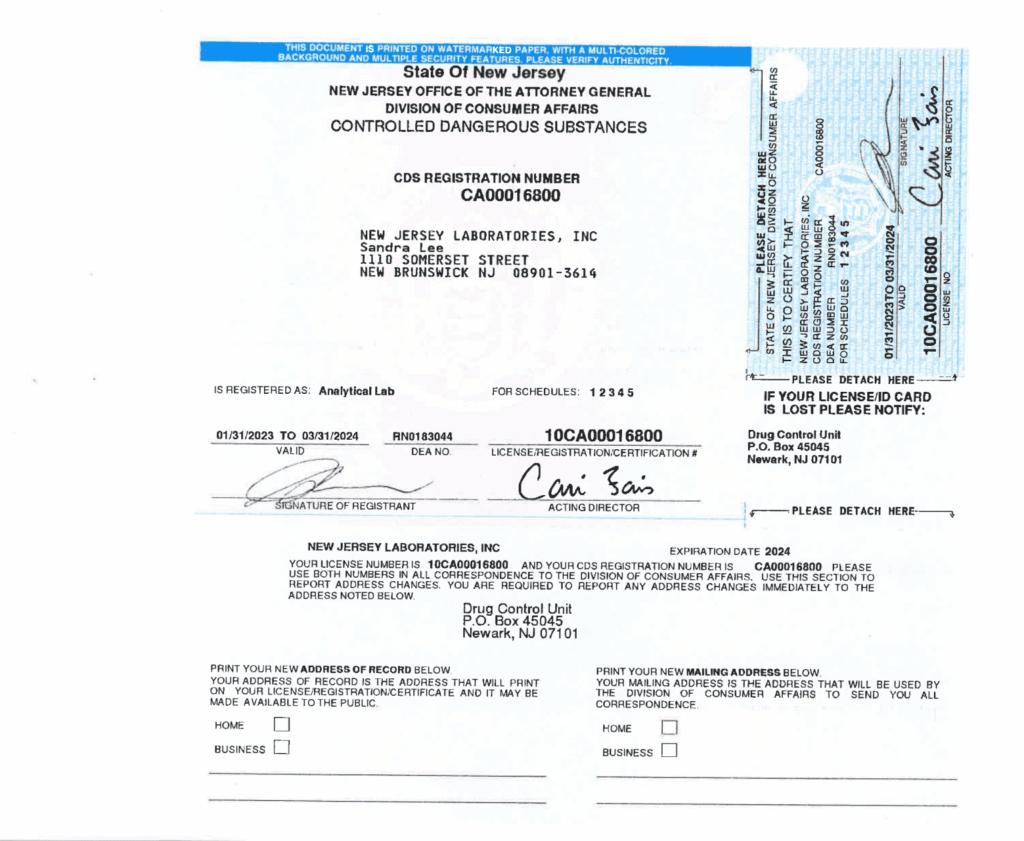
* **Application Form:** Complete the DEA Form 224, which is the application for registration under the Controlled Substances Act. This form requires detailed information about your practice, including your name, address, and the types of controlled substances you intend to prescribe.
* **State Licensing:** Provide proof of your state PA license and any other relevant state-specific credentials that authorize you to prescribe controlled substances. The DEA requires verification of your state credentials before processing your application.
* **Supervising Physician Information:** Include information about your supervising physician, including their DEA registration number and a copy of the supervisory agreement outlining your prescriptive authority. This demonstrates that you are practicing under appropriate medical supervision.
* **Background Check:** Be prepared for a background check as part of the application process. The DEA conducts background checks to ensure that applicants have not been convicted of any drug-related crimes or have a history of substance abuse.
* **Application Fee:** Pay the required application fee. The fee varies depending on the type of registration and is subject to change.
* **Submission and Processing:** Submit the completed application form and all required documentation to the DEA. The processing time can vary, so it’s essential to apply well in advance of when you need to prescribe controlled substances.
It is important to note that the DEA may conduct inspections of your practice site as part of the application process. Be prepared to demonstrate that you have adequate security measures in place to prevent diversion of controlled substances.
The Role of EPCS (Electronic Prescribing of Controlled Substances)
Electronic Prescribing of Controlled Substances (EPCS) is becoming increasingly important and, in many cases, mandatory. It represents a significant advancement in patient safety and reduces the risk of prescription fraud and diversion. EPCS allows prescribers to electronically transmit prescriptions for controlled substances directly to pharmacies, eliminating the need for paper prescriptions.
* **Enhanced Security:** EPCS offers enhanced security compared to traditional paper prescriptions. Electronic prescriptions are less susceptible to tampering and forgery, reducing the risk of fraudulent prescriptions being filled.
* **Reduced Errors:** EPCS can help reduce prescribing errors by providing access to patient medication histories and drug interaction information. This allows prescribers to make more informed decisions and avoid potentially harmful drug combinations.
* **Improved Efficiency:** EPCS streamlines the prescribing process, saving time for both prescribers and pharmacists. Electronic prescriptions can be transmitted quickly and easily, eliminating the need for phone calls and faxes.
* **Compliance with Mandates:** Many states have implemented mandates requiring EPCS for all controlled substance prescriptions. It’s essential for PAs to be aware of these mandates and ensure compliance to avoid penalties.
To implement EPCS, PAs must use certified software that meets DEA requirements. This software must include features such as identity proofing, two-factor authentication, and audit trails. PAs must also undergo training on how to use the software and comply with EPCS regulations. The DEA provides resources and guidance on EPCS implementation, including a list of certified software vendors.
Maintaining Compliance: Record Keeping and Inventory Management
Maintaining compliance with DEA regulations is an ongoing responsibility. Accurate record-keeping and proper inventory management are crucial for preventing diversion and ensuring accountability. Here are some key aspects of compliance:
* **Prescription Records:** Maintain accurate and complete records of all controlled substance prescriptions. These records should include the patient’s name, address, date of birth, the drug name, strength, dosage, quantity, and the date the prescription was issued. Keep these records readily available for inspection by the DEA.
* **Inventory Records:** Conduct regular inventories of all controlled substances in your possession. These inventories should be conducted at least every two years, but more frequent inventories are recommended. Keep detailed records of the date, time, and results of each inventory.
* **Receiving Records:** Maintain records of all controlled substances received from suppliers. These records should include the date of receipt, the supplier’s name and address, the drug name, strength, dosage, and quantity. Verify that the received drugs match the order and report any discrepancies to the DEA.
* **Disposal Records:** Properly dispose of any expired or unused controlled substances in accordance with DEA regulations. Maintain detailed records of the disposal, including the date, method of disposal, and the names of the individuals who witnessed the disposal. Many pharmacies and collection sites offer disposal services.
* **Security Measures:** Implement security measures to prevent theft and diversion of controlled substances. This may include storing controlled substances in a locked cabinet or safe, limiting access to authorized personnel, and using surveillance cameras.
Regular self-audits can help identify potential compliance issues before they become problems. Consider implementing a system for tracking prescriptions and inventories to ensure accuracy and prevent errors. Consulting with a legal professional or compliance expert can also provide valuable guidance.
Navigating State-Specific Regulations for PA Prescribing
While the DEA sets federal regulations, individual states have their own laws governing PA prescribing of controlled substances. These state regulations can vary significantly and often impose additional restrictions or requirements. It is absolutely critical for PAs to understand and comply with the specific regulations in the state(s) where they practice.
* **Scope of Practice:** State laws define the scope of practice for PAs, including the types of controlled substances they are authorized to prescribe. Some states may restrict PAs from prescribing certain Schedule II drugs or require specific training or certifications for prescribing controlled substances.
* **Supervisory Agreements:** State laws often require PAs to practice under the supervision of a licensed physician. The supervisory agreement outlines the responsibilities of the PA and the supervising physician, including the scope of prescribing authority. Review your supervisory agreement regularly to ensure it complies with state regulations.
* **Prescription Monitoring Programs (PMPs):** Most states have Prescription Monitoring Programs (PMPs) that track the prescribing and dispensing of controlled substances. PAs are typically required to register with the PMP and check the system before prescribing controlled substances to patients. PMPs help identify patients who may be at risk of drug abuse or diversion.
* **Continuing Education Requirements:** Many states require PAs to complete continuing education courses on controlled substance prescribing and pain management. These courses help PAs stay up-to-date on the latest regulations and best practices.
To stay informed about state-specific regulations, consult your state’s medical board or PA association. These organizations provide resources and guidance on PA prescribing laws. Attend continuing education courses on controlled substance prescribing to ensure you are up-to-date on the latest regulations. Engage with other PAs in your state to share information and best practices.
Addressing Common Challenges and Pitfalls
Even with a thorough understanding of DEA regulations, PAs may encounter challenges in their prescribing practices. Here are some common pitfalls to avoid:
* **Lack of Awareness:** Failing to stay informed about changes in DEA regulations and state laws. Subscribe to newsletters from the DEA and your state medical board to stay up-to-date on the latest developments.
* **Inadequate Documentation:** Maintaining incomplete or inaccurate prescription records. Implement a system for tracking prescriptions and inventories to ensure accuracy and prevent errors. Regularly review your records to identify and correct any errors.
* **Improper Disposal:** Failing to properly dispose of expired or unused controlled substances. Utilize authorized disposal methods, such as take-back programs or mail-back services. Keep detailed records of all disposals.
* **Over-Prescribing:** Prescribing excessive quantities of controlled substances or prescribing them for non-medical purposes. Adhere to established guidelines for prescribing controlled substances and monitor patients closely for signs of drug abuse or diversion.
* **Failure to Utilize PMPs:** Not checking Prescription Monitoring Programs (PMPs) before prescribing controlled substances. Use PMPs to identify patients who may be at risk of drug abuse or diversion. Share information with other healthcare providers to coordinate care and prevent drug abuse.
By addressing these common challenges and pitfalls, PAs can minimize the risk of non-compliance and ensure the safety of their patients. Proactive education and vigilance are key to responsible prescribing practices.
The Future of DEA Regulations and PA Prescribing
The landscape of DEA regulations and PA prescribing is constantly evolving. Several trends are shaping the future of this field:
* **Increased Focus on EPCS:** The adoption of EPCS is expected to continue to grow, with more states implementing mandates requiring electronic prescribing of controlled substances. This will enhance security, reduce errors, and improve efficiency in the prescribing process.
* **Expansion of PMP Use:** Prescription Monitoring Programs (PMPs) are becoming increasingly sophisticated and integrated with electronic health records. This will allow healthcare providers to access real-time data on patient medication histories and identify potential drug abuse or diversion more effectively.
* **Greater Emphasis on Pain Management:** There is a growing emphasis on non-opioid pain management strategies. PAs are encouraged to explore alternative treatments for pain, such as physical therapy, acupuncture, and cognitive behavioral therapy. Opioids should be reserved for cases where other treatments have failed.
* **Enhanced Collaboration:** Collaboration between PAs, physicians, pharmacists, and other healthcare providers is becoming increasingly important in managing controlled substances. Sharing information and coordinating care can help prevent drug abuse and diversion.
Staying informed about these trends and adapting to changes in DEA regulations is essential for PAs to provide safe and effective patient care. Continuous learning and professional development are key to navigating the evolving landscape of controlled substance prescribing.
[Product/Service Explanation – Placeholder]
[This section is a placeholder for a product or service explanation relevant to DEA compliance for Physician Assistants. For example, it could describe a specific EPCS software, a DEA compliance training program, or a service that helps PAs manage their DEA registration and renewals. The content should be tailored to fit the overall theme of the article and provide valuable information to the reader.]
[Detailed Features Analysis – Placeholder]
[This section is a placeholder for a detailed features analysis of the product or service mentioned above. It should enumerate and elaborate on at least 5-7 key features, explaining what each feature is, how it works, the specific user benefit, and how it demonstrates quality or expertise in its design/function related to DEA compliance. Provide practical examples or use cases.]
[Advantages, Benefits & Real-World Value – Placeholder]
[This section is a placeholder for the significant advantages, benefits, and real-world value of the product or service. Focus on tangible and intangible benefits that directly address user needs or solve problems. Articulate what makes the product/service superior or unique. Frame advantages with phrases suggesting experience or evidence.]
[Comprehensive & Trustworthy Review – Placeholder]
[This section is a placeholder for a comprehensive and trustworthy review of the product or service. Provide a balanced perspective, detailing user experience, usability, and performance. List pros and cons, identify the ideal user profile, and mention key alternatives. Conclude with a clear, authoritative recommendation.]
Insightful Q&A Section: Common Questions About DEA for Physician Assistant
Here are some frequently asked questions regarding DEA regulations for physician assistants:
1. **Q: Can a PA prescribe Schedule I controlled substances?**
A: No, Schedule I controlled substances have no accepted medical use and cannot be prescribed by any practitioner, including PAs.
2. **Q: How often do I need to renew my DEA registration?**
A: DEA registration must be renewed every three years. The DEA will send a renewal notice approximately 60 days before the expiration date.
3. **Q: What should I do if my DEA registration is lost or stolen?**
A: Immediately report the loss or theft to the DEA and file a police report. You will need to apply for a duplicate registration.
4. **Q: Can I prescribe controlled substances in states where I am not licensed?**
A: No, you can only prescribe controlled substances in states where you hold a valid PA license and DEA registration.
5. **Q: What are the penalties for violating DEA regulations?**
A: Penalties for violating DEA regulations can include fines, imprisonment, and revocation of your DEA registration and PA license.
6. **Q: How do I dispose of unused controlled substances properly?**
A: You can dispose of unused controlled substances through authorized take-back programs, mail-back services, or by transferring them to a registered reverse distributor.
7. **Q: What is the role of the supervising physician in PA prescribing of controlled substances?**
A: The supervising physician is responsible for overseeing the PA’s prescribing practices and ensuring compliance with DEA regulations and state laws.
8. **Q: Are there any limitations on the quantity of controlled substances I can prescribe?**
A: State laws may impose limitations on the quantity of controlled substances you can prescribe. Check your state’s regulations for specific limits.
9. **Q: How can I stay updated on changes in DEA regulations and state laws?**
A: Subscribe to newsletters from the DEA and your state medical board. Attend continuing education courses on controlled substance prescribing.
10. **Q: What is the best way to document controlled substance prescriptions in the patient’s medical record?**
A: Document the patient’s name, address, date of birth, the drug name, strength, dosage, quantity, and the date the prescription was issued. Also, document the medical necessity for the prescription and any relevant clinical information.
Conclusion: Mastering DEA Compliance for Physician Assistant Practice
Navigating the complexities of DEA regulations is essential for physician assistants who prescribe controlled substances. By understanding the requirements for registration, compliance, and responsible prescribing practices, PAs can ensure the safety of their patients and avoid potential legal issues. This comprehensive guide has provided a detailed overview of the key aspects of DEA compliance, empowering you to confidently manage controlled substances within your practice.
Remember to stay informed about changes in DEA regulations and state laws, maintain accurate records, and prioritize patient safety. By adhering to these principles, you can provide high-quality care while maintaining compliance with the law. Share your experiences with DEA compliance in the comments below. Explore our advanced guide to pain management for additional insights. Contact our experts for a consultation on DEA compliance best practices.