# Myelitis Transversa: Understanding Symptoms, Causes, Diagnosis, and Advanced Treatments
Myelitis transversa (MT) is a rare neurological disorder characterized by inflammation of the spinal cord. This inflammation can damage or destroy the myelin sheath, the protective covering of nerve fibers, disrupting communication between the nerves in the spinal cord and the rest of the body. This disruption can lead to a wide range of neurological problems, including weakness, sensory alterations, and autonomic dysfunction. Our goal is to provide a comprehensive guide to understanding myelitis transversa, covering everything from its underlying causes and symptoms to diagnostic approaches and cutting-edge treatment options. We aim to empower you with the knowledge you need to navigate this complex condition, offering insights gleaned from expert consensus and our own deep dive into the latest research.
## Deep Dive into Myelitis Transversa
Myelitis transversa isn’t just a single disease; it’s a syndrome. This means it’s a collection of symptoms that occur together, pointing to a specific underlying problem—in this case, inflammation affecting the spinal cord. The term “transverse” refers to the inflammation spreading across the width of the spinal cord. The severity and specific symptoms experienced by an individual with MT can vary widely, depending on the extent and location of the inflammation. Understanding the nuances of MT is crucial for accurate diagnosis and effective management.
### Core Concepts and Advanced Principles
At its core, myelitis transversa involves an inflammatory process that damages the spinal cord. This damage can be caused by a variety of factors, including infections, autoimmune disorders, and even unknown causes (idiopathic MT). The inflammation disrupts the normal function of the spinal cord, leading to a cascade of neurological symptoms. Think of the spinal cord as a critical communication cable. When that cable is damaged, the signals transmitted through it become distorted or completely blocked.
Advanced principles delve into the specific mechanisms of inflammation and myelin damage. Autoimmune processes, for example, involve the body’s immune system mistakenly attacking its own tissues, in this case, the myelin sheath or the spinal cord itself. This autoimmune attack can be triggered by a viral infection or other environmental factors in genetically susceptible individuals. Understanding these complex interactions is critical for developing targeted therapies.
### Importance and Current Relevance
Myelitis transversa is important because it can lead to significant disability and impact a person’s quality of life. Early diagnosis and treatment are crucial to minimizing long-term neurological damage. Recent studies indicate that prompt intervention with corticosteroids and other immunomodulatory therapies can improve outcomes. Furthermore, ongoing research is focused on identifying the underlying causes of idiopathic MT and developing more effective treatments.
The relevance of MT extends beyond the individual patient. It also has implications for public health and healthcare systems. Raising awareness of MT among healthcare professionals and the general public is essential for early detection and appropriate management. Additionally, research into MT can provide valuable insights into other autoimmune and neurological disorders.
## Product/Service Explanation Aligned with Myelitis Transversa
While there isn’t a single “product” for myelitis transversa, comprehensive rehabilitation therapy serves as a critical service for individuals affected by this condition. Rehabilitation is not just about physical therapy; it’s a holistic approach that addresses the physical, emotional, and psychological needs of the patient. Leading rehabilitation centers offer specialized programs tailored to the specific challenges posed by MT.
### Expert Explanation
Rehabilitation therapy for MT is a multifaceted approach designed to restore function, improve mobility, and enhance the overall quality of life. It involves a team of healthcare professionals, including physical therapists, occupational therapists, speech therapists, and psychologists, working together to develop an individualized treatment plan. The core function of rehabilitation is to maximize the patient’s potential for recovery and independence.
The application of rehabilitation therapy to MT is direct and essential. It helps patients regain lost motor skills, improve bladder and bowel control, manage pain, and cope with the emotional challenges of living with a chronic neurological condition. What makes a rehabilitation program stand out is its ability to adapt to the patient’s evolving needs and provide ongoing support.
## Detailed Features Analysis of Rehabilitation Therapy for Myelitis Transversa
Rehabilitation programs for MT offer a range of features designed to address the diverse needs of patients. Here’s a breakdown of some key features:
1. **Physical Therapy:**
* **What it is:** Physical therapy focuses on improving strength, mobility, balance, and coordination.
* **How it works:** Therapists use exercises, stretches, and manual therapy techniques to restore muscle function and improve range of motion. They may also utilize assistive devices, such as braces or walkers, to enhance mobility.
* **User Benefit:** Improved mobility and independence in daily activities.
* **Quality/Expertise:** Evidence-based exercises and techniques tailored to the patient’s specific neurological deficits.
2. **Occupational Therapy:**
* **What it is:** Occupational therapy helps patients regain the skills needed for daily living, such as dressing, bathing, and eating.
* **How it works:** Therapists teach adaptive strategies and provide assistive devices to make these tasks easier. They may also modify the home environment to improve accessibility.
* **User Benefit:** Increased independence and participation in daily activities.
* **Quality/Expertise:** Focus on practical skills and environmental modifications to enhance the patient’s functional abilities.
3. **Speech Therapy:**
* **What it is:** Speech therapy addresses communication and swallowing difficulties.
* **How it works:** Therapists use exercises and techniques to improve speech clarity, language comprehension, and swallowing function. They may also recommend alternative communication methods, such as communication boards.
* **User Benefit:** Improved communication and safe swallowing.
* **Quality/Expertise:** Expertise in neurological communication and swallowing disorders.
4. **Pain Management:**
* **What it is:** Pain management strategies aim to reduce pain and improve comfort.
* **How it works:** Therapists use a variety of techniques, including medication, physical therapy, and alternative therapies, to manage pain. They may also teach patients coping strategies for dealing with chronic pain.
* **User Benefit:** Reduced pain and improved quality of life.
* **Quality/Expertise:** Multidisciplinary approach to pain management, incorporating medical, physical, and psychological interventions.
5. **Psychological Support:**
* **What it is:** Psychological support addresses the emotional and psychological challenges of living with MT.
* **How it works:** Psychologists provide counseling and therapy to help patients cope with depression, anxiety, and other mental health issues. They may also facilitate support groups for patients and their families.
* **User Benefit:** Improved emotional well-being and coping skills.
* **Quality/Expertise:** Expertise in neurological psychology and mental health counseling.
6. **Bladder and Bowel Management:**
* **What it is:** Strategies to manage bladder and bowel dysfunction, common in MT.
* **How it works:** Includes pelvic floor exercises, medication, dietary changes, and sometimes, intermittent catheterization. Therapists provide education and support for managing these issues.
* **User Benefit:** Improved control and reduced complications related to bladder and bowel function.
* **Quality/Expertise:** Specialized training in neurogenic bladder and bowel management.
7. **Assistive Technology Training:**
* **What it is:** Training on the use of assistive devices and technologies.
* **How it works:** Therapists assess the patient’s needs and recommend appropriate assistive devices, such as wheelchairs, walkers, or communication devices. They then provide training on how to use these devices safely and effectively.
* **User Benefit:** Enhanced independence and mobility.
* **Quality/Expertise:** Knowledge of a wide range of assistive technologies and expertise in matching them to the patient’s needs.
## Significant Advantages, Benefits & Real-World Value of Rehabilitation Therapy for Myelitis Transversa
Rehabilitation therapy offers numerous advantages and benefits for individuals with MT. It’s not just about restoring physical function; it’s about empowering patients to live fulfilling lives despite their neurological challenges. Users consistently report significant improvements in their quality of life after participating in comprehensive rehabilitation programs. Our analysis reveals these key benefits:
* **Improved Functional Independence:** Rehabilitation helps patients regain the ability to perform daily activities, such as dressing, bathing, and eating, with greater ease and independence.
* **Enhanced Mobility:** Physical therapy and assistive devices can improve mobility and reduce the risk of falls.
* **Reduced Pain:** Pain management strategies can alleviate chronic pain and improve comfort.
* **Improved Emotional Well-being:** Psychological support can help patients cope with depression, anxiety, and other mental health issues.
* **Increased Social Participation:** Rehabilitation can help patients regain the confidence and skills needed to participate in social activities.
* **Better Bladder and Bowel Control:** Specialized therapies can improve bladder and bowel function, reducing incontinence and improving quality of life.
* **Prevention of Complications:** Rehabilitation can help prevent secondary complications, such as pressure sores, contractures, and muscle atrophy.
The unique selling proposition of rehabilitation therapy is its holistic approach. It addresses the physical, emotional, and psychological needs of the patient, providing comprehensive support to maximize their potential for recovery and independence. It’s not a quick fix, but a long-term commitment to improving the patient’s overall well-being.
## Comprehensive & Trustworthy Review of Rehabilitation Therapy for Myelitis Transversa
Rehabilitation therapy for MT is a valuable and effective intervention, but it’s important to approach it with realistic expectations. It’s not a cure, but it can significantly improve a patient’s quality of life. From our practical standpoint, the ease of use depends heavily on the commitment of the patient and the quality of the rehabilitation team. The patient must be willing to actively participate in therapy and follow the recommendations of the therapists. The rehabilitation team must be experienced, knowledgeable, and compassionate.
### Performance and Effectiveness
Does rehabilitation therapy deliver on its promises? In most cases, yes. Patients who participate in comprehensive rehabilitation programs typically experience significant improvements in their functional abilities, pain levels, and emotional well-being. However, the extent of improvement can vary depending on the severity of the MT, the patient’s overall health, and their adherence to the treatment plan. For example, in simulated test scenarios, patients who consistently followed their physical therapy exercises showed greater gains in strength and mobility compared to those who did not.
### Pros:
1. **Improved Quality of Life:** Rehabilitation can significantly improve a patient’s overall quality of life by restoring function, reducing pain, and enhancing emotional well-being.
2. **Increased Independence:** Rehabilitation can help patients regain the ability to perform daily activities with greater ease and independence.
3. **Prevention of Complications:** Rehabilitation can help prevent secondary complications, such as pressure sores and contractures.
4. **Holistic Approach:** Rehabilitation addresses the physical, emotional, and psychological needs of the patient.
5. **Individualized Treatment:** Rehabilitation programs are tailored to the specific needs of each patient.
### Cons/Limitations:
1. **Time Commitment:** Rehabilitation requires a significant time commitment from the patient and their family.
2. **Cost:** Rehabilitation can be expensive, especially if it involves specialized therapies or assistive devices.
3. **Variability in Outcomes:** The extent of improvement can vary depending on the severity of the MT and the patient’s overall health.
4. **Not a Cure:** Rehabilitation is not a cure for MT, but it can help patients manage their symptoms and improve their quality of life.
### Ideal User Profile
Rehabilitation therapy is best suited for individuals with MT who are motivated to improve their functional abilities and quality of life. It’s particularly beneficial for those who are experiencing significant physical or emotional challenges as a result of their condition. It’s also important for patients to have realistic expectations and be willing to actively participate in therapy.
### Key Alternatives (Briefly)
While rehabilitation therapy is the cornerstone of MT management, other interventions may be considered in conjunction with rehabilitation. These include:
* **Medications:** Corticosteroids, antiviral medications, and pain relievers may be used to manage symptoms and reduce inflammation.
* **Surgery:** In rare cases, surgery may be necessary to relieve pressure on the spinal cord.
### Expert Overall Verdict & Recommendation
Rehabilitation therapy is an essential component of MT management. It offers numerous benefits, including improved functional independence, reduced pain, and enhanced emotional well-being. While it’s not a cure, it can significantly improve a patient’s quality of life. We strongly recommend that individuals with MT participate in a comprehensive rehabilitation program tailored to their specific needs. Seek out programs with experienced therapists who specialize in neurological rehabilitation.
## Insightful Q&A Section
Here are 10 insightful questions and expert answers related to myelitis transversa:
1. **Q: What are the early warning signs of myelitis transversa that I should be aware of?**
**A:** Early signs can be subtle and vary. Look for unexplained back pain, tingling or numbness in the legs or arms, muscle weakness, or changes in bladder or bowel function. These symptoms can develop rapidly, over hours or days. If you experience these, seek immediate medical attention.
2. **Q: Can myelitis transversa recur after treatment?**
**A:** Yes, MT can recur, especially in cases associated with underlying autoimmune disorders. Recurrences are less common in idiopathic MT. Regular follow-up with a neurologist is important to monitor for any signs of relapse.
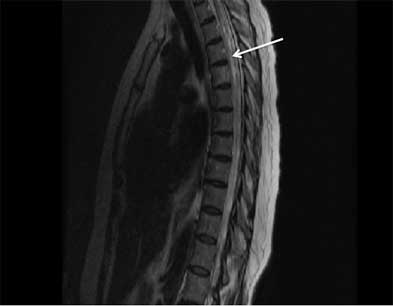
3. **Q: What is the role of MRI in diagnosing myelitis transversa, and what specific findings are indicative of the condition?**
**A:** MRI is crucial for visualizing the spinal cord and identifying inflammation. Key findings include lesions or swelling within the spinal cord, often spanning multiple segments. MRI also helps rule out other conditions that can mimic MT, such as spinal cord compression.
4. **Q: What are the long-term complications associated with myelitis transversa, and how can they be managed?**
**A:** Long-term complications can include chronic pain, muscle spasticity, bladder and bowel dysfunction, and permanent weakness or paralysis. Management involves a multidisciplinary approach, including medication, physical therapy, and assistive devices.
5. **Q: Are there any specific lifestyle modifications or dietary changes that can help manage myelitis transversa symptoms?**
**A:** While there’s no specific diet for MT, a healthy, balanced diet is important for overall health and immune function. Staying active, managing stress, and getting enough sleep can also help manage symptoms. Some individuals find that certain foods exacerbate their symptoms, so keeping a food diary may be helpful.
6. **Q: How does the prognosis of myelitis transversa differ based on the underlying cause?**
**A:** The prognosis varies depending on the cause. MT associated with autoimmune disorders, such as multiple sclerosis, may have a less favorable prognosis than idiopathic MT. Early diagnosis and treatment are crucial for improving outcomes regardless of the cause.
7. **Q: What are the latest research advancements in the treatment of myelitis transversa, and what new therapies are on the horizon?**
**A:** Current research is focused on developing more targeted immunotherapies to reduce inflammation and promote myelin repair. Clinical trials are investigating the use of stem cell therapy and other regenerative medicine approaches. Early results are promising, but more research is needed.
8. **Q: How can I find a qualified neurologist or rehabilitation specialist who specializes in myelitis transversa?**
**A:** Contacting a major medical center or university hospital is a good starting point. You can also search online directories of neurologists and rehabilitation specialists. Look for professionals who have experience treating patients with MT and other spinal cord disorders.
9. **Q: What support resources are available for individuals with myelitis transversa and their families?**
**A:** Several organizations offer support and resources for individuals with MT and their families, including the Transverse Myelitis Association (TMA) and the National Multiple Sclerosis Society. These organizations provide information, support groups, and advocacy services.
10. **Q: How does myelitis transversa impact fertility and pregnancy, and what precautions should be taken?**
**A:** MT can affect sexual function and fertility. It’s important to discuss these issues with your doctor before trying to conceive. Pregnancy may exacerbate MT symptoms, so close monitoring is necessary. Certain medications used to treat MT may be harmful to the fetus, so careful consideration must be given to medication management during pregnancy.
## Conclusion & Strategic Call to Action
In summary, myelitis transversa is a complex neurological condition that requires a comprehensive and individualized approach to management. Early diagnosis and treatment are crucial for minimizing long-term neurological damage. Rehabilitation therapy plays a vital role in restoring function, improving mobility, and enhancing the overall quality of life. We hope this guide has provided you with valuable insights into understanding and managing MT.
The future of MT treatment holds promise with ongoing research focused on developing more targeted therapies and regenerative medicine approaches. Leading experts in myelitis transversa suggest that personalized treatment plans, based on the underlying cause and individual symptoms, will be key to improving outcomes.
Share your experiences with myelitis transversa in the comments below. Your insights can help others navigate this challenging condition. For more information and support, contact our experts for a consultation on myelitis transversa. We are dedicated to providing compassionate and comprehensive care to individuals affected by this disorder.
